Healthcare is evolving beyond traditional walls, and at the forefront of this revolution stands a new breed of medical professional: community paramedics. As emergency departments face overcrowding and rural areas struggle with healthcare access, community paramedics are filling crucial gaps by bringing care directly to patients’ homes. This article focuses on all of the distinct prerequisites, certifications, education, and more required in community paramedic training.
For medical professionals seeking meaningful career advancement, community paramedicine represents one of healthcare’s most dynamic and rapidly growing specialties—offering both expanded clinical responsibilities and the profound satisfaction of serving vulnerable populations outside traditional settings.
Understanding Community Paramedicine
Community paramedicine represents an innovative extension of traditional emergency medical services, transforming paramedics into healthcare providers who deliver non-emergency, preventive care directly in community settings. This model emerged as healthcare systems recognized the need to address gaps in service delivery, particularly in rural and underserved areas where medical resources are limited.
The evolution of community paramedicine reflects a natural progression in emergency medical services:
- Origins: Began in rural areas where paramedics provided basic preventive services to compensate for physician shortages
- Development: Expanded to urban environments focusing on reducing emergency department visits and hospital readmissions
- Current state: Now encompasses chronic disease monitoring, medication management, post-hospital discharge follow-up, and preventive care
Recent data demonstrates the effectiveness of this approach, with community paramedicine programs showing a reduction in emergency department visits by 21% to nearly 59% compared to traditional EMS pathways. These programs have also significantly reduced hospital readmissions through post-discharge care and chronic disease monitoring for high-risk patients.
Distinction Between Community Paramedicine and Mobile Integrated Healthcare
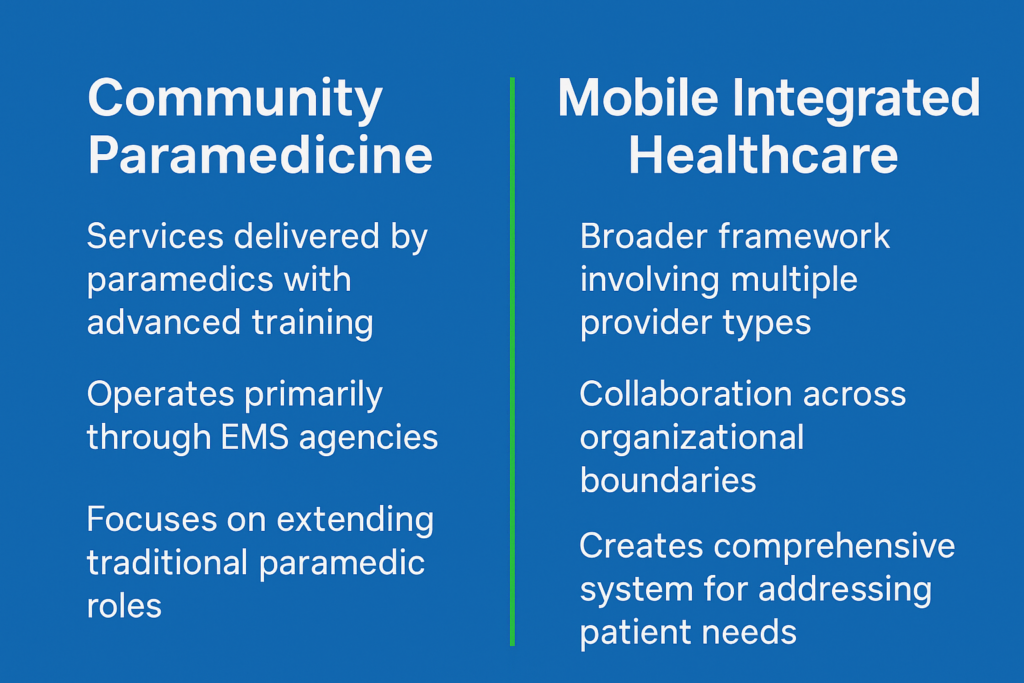
While the terms are sometimes used interchangeably, community paramedicine and mobile integrated healthcare (MIH) represent distinct but overlapping concepts:
Both models share the common goal of improving patient outcomes while reducing healthcare costs, but they differ in their organizational structure and the breadth of services provided. Understanding this distinction is essential for healthcare professionals considering career paths in this evolving field.
Role and Responsibilities of a Community Paramedic
The community paramedic scope of practice represents a significant evolution of the traditional paramedic’s role, expanding beyond emergency response to encompass preventive care, chronic disease management, and healthcare coordination.
Daily Duties and Scope of Practice
Community paramedics perform a diverse range of clinical and supportive services:
- Health assessment: Conducting comprehensive in-home health evaluations
- Chronic disease management: Monitoring vital signs and medication adherence for conditions like heart failure or diabetes
- Patient education: Teaching self-management skills for conditions like COPD or diabetes
- Care coordination: Serving as liaisons between patients and their healthcare providers
- Post-discharge monitoring: Ensuring patients understand discharge instructions and helping prevent readmissions
This expanded scope has demonstrated significant economic benefits, including a reduction in ED transportation by approximately half, a major driver of cost savings for healthcare systems. Programs have achieved returns on investment ranging from 20% to substantial annual cost savings per patient.
Work Settings for Community Paramedics
Community paramedics operate across diverse environments:
- Patients’ homes: Primary workplace allowing personalized assessment of living conditions
- Integrated healthcare systems: Collaboration with primary care practices, hospitals, and specialty clinics
- Rural and underserved communities: Addressing significant healthcare access challenges through mobile clinics and community outreach
- Telehealth platforms: Using technology to extend reach and collaborate with distant healthcare providers
Case Study: Quapaw Nation Community Paramedicine Program:
This innovative program in rural Oklahoma demonstrates the effectiveness of community paramedicine in tribal settings. Founded two years ago by EMS professional Kyle Arnall, the program serves tribal elders through home visits, medical appointment transportation, medication delivery, and air quality monitoring. The program’s patient-centered approach has resulted in a 17% reduction in 911 calls throughout the county, faster emergency response times, and improved health outcomes for tribal elders.
Education and Training Pathways
Pursuing a career as a community paramedic requires additional specialized education beyond standard paramedic training. This advanced preparation equips practitioners with the expanded clinical knowledge and patient-centered skills necessary to deliver comprehensive care in community settings.
Required Educational Background
The foundation for any community paramedic program begins with:
- Current, unrestricted paramedic license
- Typically 2+ years of full-time field experience (or equivalent part-time experience)
- Often some college-level coursework, particularly in subjects relevant to healthcare delivery
- Meeting all jurisdictional requirements, which vary by state and region
Key Training Programs and Courses
Community paramedic training programs typically follow a standardized curriculum combining classroom instruction with clinical practice:
- Didactic component: Approximately 114 hours covering chronic disease management, social determinants of health, preventive care strategies, and interprofessional collaboration
- Clinical component: About 196 hours of supervised practice in various healthcare settings
- Specialized courses: Addressing specific population health needs such as geriatric care, mental health interventions, and substance use disorders
- Capstone project: Final training component involving care plan development and implementation for high-risk patients
Certification and Licensure Requirements
After completing an accredited program, graduates must obtain proper certification:
- International Board of Specialty Certification (IBSC): Offers the Community Paramedic Certification (CP-C) examination
- Certification maintenance: Requires approximately 12 hours of approved continuing education annually
- State-specific requirements: May include formal endorsement programs or operation under existing paramedic licenses with medical director approval
Admission and Enrollment Considerations
Navigating the path to becoming a community paramedic requires careful consideration of educational options and prerequisites. Understanding admission requirements and program selection criteria has become increasingly important for prospective students seeking to advance their careers.
Prerequisites for Community Paramedic Training
Most programs maintain strict prerequisites:
- Current, unrestricted EMT or paramedic certification/license in good standing
- 1-3 years of active field practice as a paramedic
- Educational requirements ranging from high school diploma to associate degree
- Additional certifications such as ACLS, PALS, and ITLS
- Some programs require pre-admission assessments or interviews
Tips for Selecting the Right Program
When evaluating program options, consider:
- Accreditation: Look for programs approved by your state’s EMS regulatory board or aligned with IBSC guidelines
- Curriculum comprehensiveness: Balance of clinical skills with training in social determinants of health, cultural competency, and healthcare navigation
- Program format: Consider flexibility needs and whether online, in-person, or hybrid formats best fit your situation
- Faculty expertise: Research instructor qualifications and practical experience
- Graduate success: Certification pass rates and employment outcomes
Advanced Skills and Competencies
Beyond basic training, community paramedics require a sophisticated skill set that combines clinical expertise with interpersonal abilities. These advanced competencies distinguish community paramedics from traditional EMS providers and equip them to deliver effective care across diverse settings and populations.
Essential Skills for Effective Practice
Key competencies for successful community paramedics include:
- Clinical assessment in non-traditional settings: Enhanced observational abilities and critical thinking skills
- Advanced communication: Translating complex medical information for varying levels of health literacy
- Cultural competence and empathy: Building trust with diverse patient populations
- Resource navigation: Comprehensive knowledge of local healthcare and social service resources
- Technical proficiency: Comfort with electronic health records, telehealth platforms, and remote monitoring devices
Patient satisfaction with community paramedicine is consistently high, with patients particularly valuing the personalized care, health education, and convenience of receiving services at home.
Continuing Education and Skill Enhancement
Maintaining and expanding skills requires ongoing professional development:
- Continuing education: Typically 12-24 hours annually to maintain certification
- Specialized certifications: Additional credentials in areas like geriatric care or diabetes management
- Interdisciplinary learning: Workshops and courses designed for primary care providers or social workers
- Mentorship relationships: Both receiving guidance and eventually mentoring newer colleagues
- Research participation: Contributing to the field’s evidence base through quality improvement projects or formal studies
Certification Exam and Renewal
Achieving and maintaining community paramedic certification represents a crucial step in establishing yourself as a qualified professional in this specialized field. The certification process validates your advanced knowledge and skills while demonstrating your commitment to excellence.
Preparing for the CP-C Examination
The IBSC community paramedic examination (CP-C) serves as the industry standard for certifying competency. Effective preparation strategies include:
- Content mastery: Systematic review of all domains outlined in the IBSC study guide
- Practice examinations: Regular practice with timed tests to build test-taking stamina
- Structured review courses: Guided learning opportunities, particularly in the final weeks before testing
- Study groups: Collaborative preparation enabling participants to explain concepts to one another
Certification Renewal Process and Requirements
The IBSC certification remains valid for four years, after which practitioners must complete a formal renewal process:
- Continuing education pathway: Typically requires approximately 100 hours of approved education during the four-year period
- Examination pathway: Option to recertify by retaking the complete certification test
- Documentation requirements: Detailed records of all continuing education activities
- Renewal fees: Processing fees for certification renewal, which may increase after deadlines
- Professional development planning: Strategic approach to continuing education aligned with career goals
Funding and Financial Support Options
Financing advanced education in community paramedicine presents a significant challenge for many prospective students. Various funding mechanisms exist to offset these costs, including employer support, dedicated grants, and scholarship opportunities.
Avenues for Funding Education and Training
Consider these potential funding sources:
- Employer-sponsored funding: Many EMS agencies and healthcare systems invest in workforce development
- Federal workforce development grants: Particularly in rural and underserved areas
- State-level funding initiatives: Several states have allocated resources specifically for community paramedicine education
- Healthcare system partnerships: Hospitals and health insurance companies may offer educational sponsorships
- Traditional financial aid: Federal grants, loans, and work-study opportunities for eligible students
Scholarships, Grants, and Financial Aid Opportunities
Specialized funding opportunities include:
- EMS and paramedicine scholarships: Through organizations like the National Association of Emergency Medical Technicians (NAEMT)
- Foundation grants: Organizations like the Robert Wood Johnson Foundation supporting healthcare workforce development
- Rural-specific funding: Special opportunities for those planning to practice in non-urban settings
- Public service loan forgiveness: Programs that forgive remaining federal student loan balances after service in qualifying settings
- Industry partnerships: Medical equipment manufacturers, pharmaceutical companies, and healthcare technology firms sometimes establish scholarship programs
Career Outlook and Advancement
The field of community paramedicine continues to evolve rapidly, creating expanding opportunities for qualified professionals. Understanding the career landscape and advancement pathways helps professionals make informed decisions about their educational investments.
Job Market and Demand for Community Paramedics
The employment outlook remains exceptionally positive, driven by healthcare trends emphasizing preventive care and chronic disease management:
- Rural and underserved communities: Particularly strong markets addressing physician shortages
- Salary ranges: Entry-level positions typically between $44,096 and $58,507 annually according to recent compensation data, with higher earnings in urban areas
- Diverse employment settings: Expansion beyond traditional EMS agencies to healthcare systems, accountable care organizations, and home health agencies
- Emerging care models: Novel opportunities in telehealth programs and hospital-at-home initiatives
Opportunities for Professional Growth and Leadership
Advancement pathways for community paramedics include:
- Clinical specialization: Developing expertise in areas such as geriatric care or mental health intervention
- Program development and management: Designing protocols, establishing quality metrics, and overseeing operations
- Educational leadership: Serving as field training officers, clinical preceptors, or formal instructors
- Research participation: Contributing to quality improvement initiatives and formal studies
- Healthcare administration: Transitioning to system-level roles in quality improvement or healthcare policy
- Entrepreneurship: Establishing independent consulting businesses or specialized training companies
Case Study: Central Oregon Community Paramedicine Program:
This program implemented an innovative approach to address non-urgent emergency department utilization among complex Medicaid patients in rural Oregon counties. Using a rigorous scientific methodology with control groups, the program demonstrated a 14% reduction in urgent emergency department visits and 40% reduction in avoidable ED visits, providing strong evidence supporting community paramedicine in rural settings.
Frequently Asked Questions
What qualifications do I need to become a community paramedic?
At minimum, you need a current paramedic license, typically 1-3 years of field experience, and completion of a specialized community paramedicine training program (approximately 300 total hours). Some states have additional requirements.
How much do community paramedics earn?
According to recent compensation data, community paramedics earn between $44,096 and $58,507 annually, with variation based on location, experience, and employer type. Urban areas and regions with higher costs of living generally offer higher salaries.
How effective are community paramedicine programs?
Research demonstrates significant effectiveness, with programs reducing emergency department visits by 21-59% and cutting ED transportation by approximately half. Programs have shown substantial cost savings and high patient satisfaction rates.
What’s the difference between a community paramedic and a regular paramedic?
Community paramedics have additional training beyond the standard paramedic curriculum, focusing on preventive care, chronic disease management, social determinants of health, and care coordination. They typically work in non-emergency settings and have a more autonomous scope of practice.
Where do community paramedics typically work?
While some work for traditional EMS agencies, many are employed by healthcare systems, hospitals, home health agencies, public health departments, accountable care organizations, and integrated health networks. They primarily provide care in patients’ homes and community settings rather than ambulances.
How do I maintain my community paramedic certification?
Certification through the International Board of Specialty Certification (IBSC) requires renewal every four years through either continuing education (approximately 100 hours over four years) or retaking the certification examination.
Conclusion
Community paramedicine represents a dynamic and rapidly evolving specialty within the emergency medical services field. For paramedics seeking to expand their clinical skills while making a meaningful difference in healthcare delivery, this career path offers exceptional opportunities for professional growth and patient impact.
The combination of specialized community paramedic training, certification, and experience opens doors to diverse practice settings and advancement pathways. As healthcare continues to shift toward preventive models focused on reducing unnecessary hospitalizations and emergency department visits, qualified community paramedics will remain in high demand across urban and rural settings alike.
By pursuing the educational requirements and advanced competencies outlined in this article, paramedics can position themselves at the forefront of healthcare innovation—bringing vital services to vulnerable populations and helping create more effective, patient-centered healthcare delivery systems.